My Experience Using a Continuous Glucose Monitor
 On 17 December I started wearing a Freestyle Libra 2 Continuous Glucose Monitor (CGM) to see the patterns of my blood glucose (BG). I timed it particularly so that the 14 days the CGM sensor lasts included Christmas. It has been an interesting and informative experience. The image shows the kit with the sensor and some patches to help with waterproofing and prevent catching on clothes - I did not use them in the end.
On 17 December I started wearing a Freestyle Libra 2 Continuous Glucose Monitor (CGM) to see the patterns of my blood glucose (BG). I timed it particularly so that the 14 days the CGM sensor lasts included Christmas. It has been an interesting and informative experience. The image shows the kit with the sensor and some patches to help with waterproofing and prevent catching on clothes - I did not use them in the end.
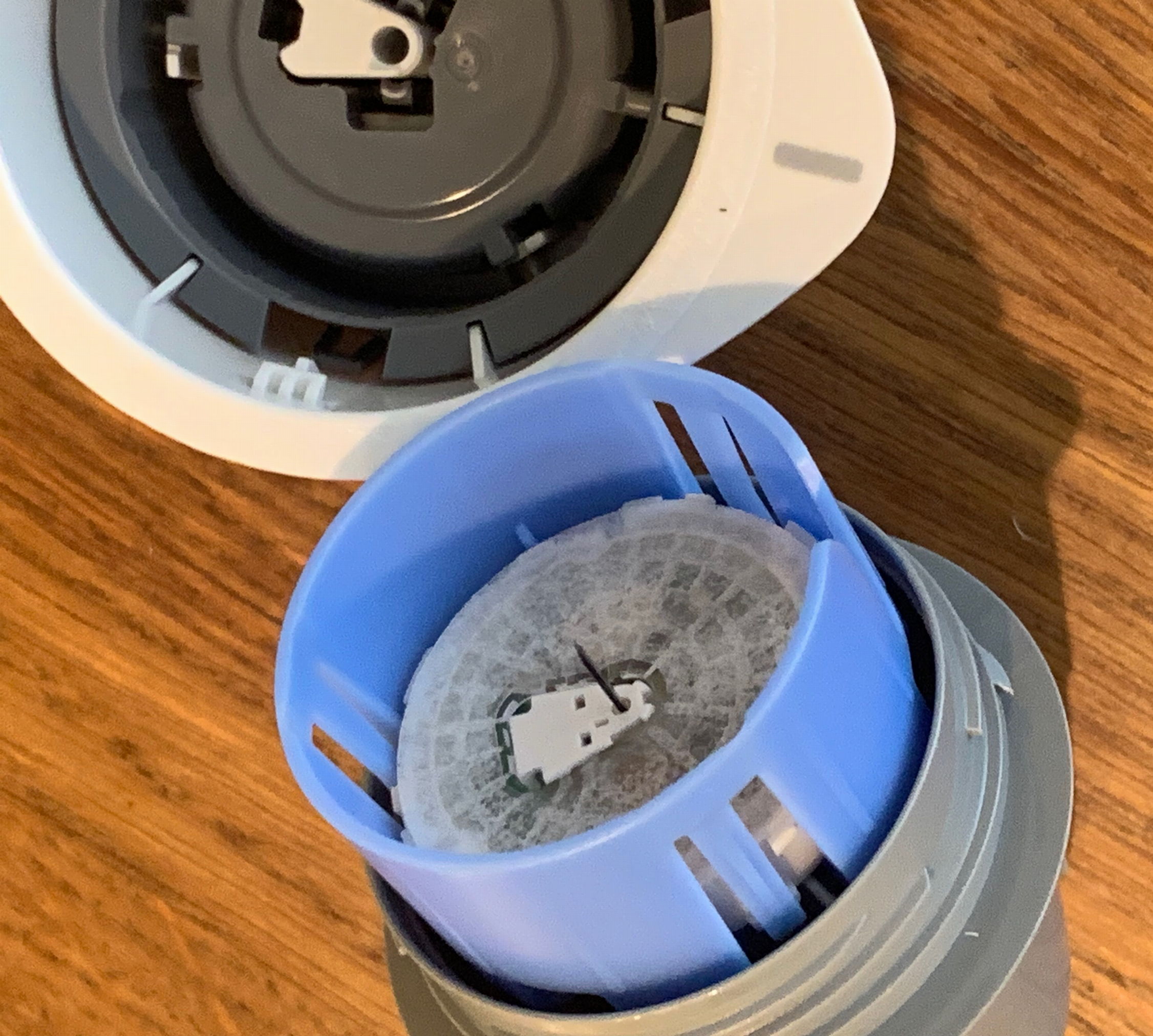 The sensor before inserting. Despite the slightly intimidating appearance, you don’t really feel the needle go in at all.
The sensor before inserting. Despite the slightly intimidating appearance, you don’t really feel the needle go in at all.

CGM is well established in the management of Type 1 and Type 2 diabetes, where they can be prescribed on the NHS. However, some GPs including, Dr David Unwin have shown them to be very useful for insulin resistant or pre-diabetic patients, as CGM allows them to learn what foods raise their blood glucose, and therefore eat something else. I was using CGM as an N=1 experiment to see how my blood glucose was faring on a keto diet.
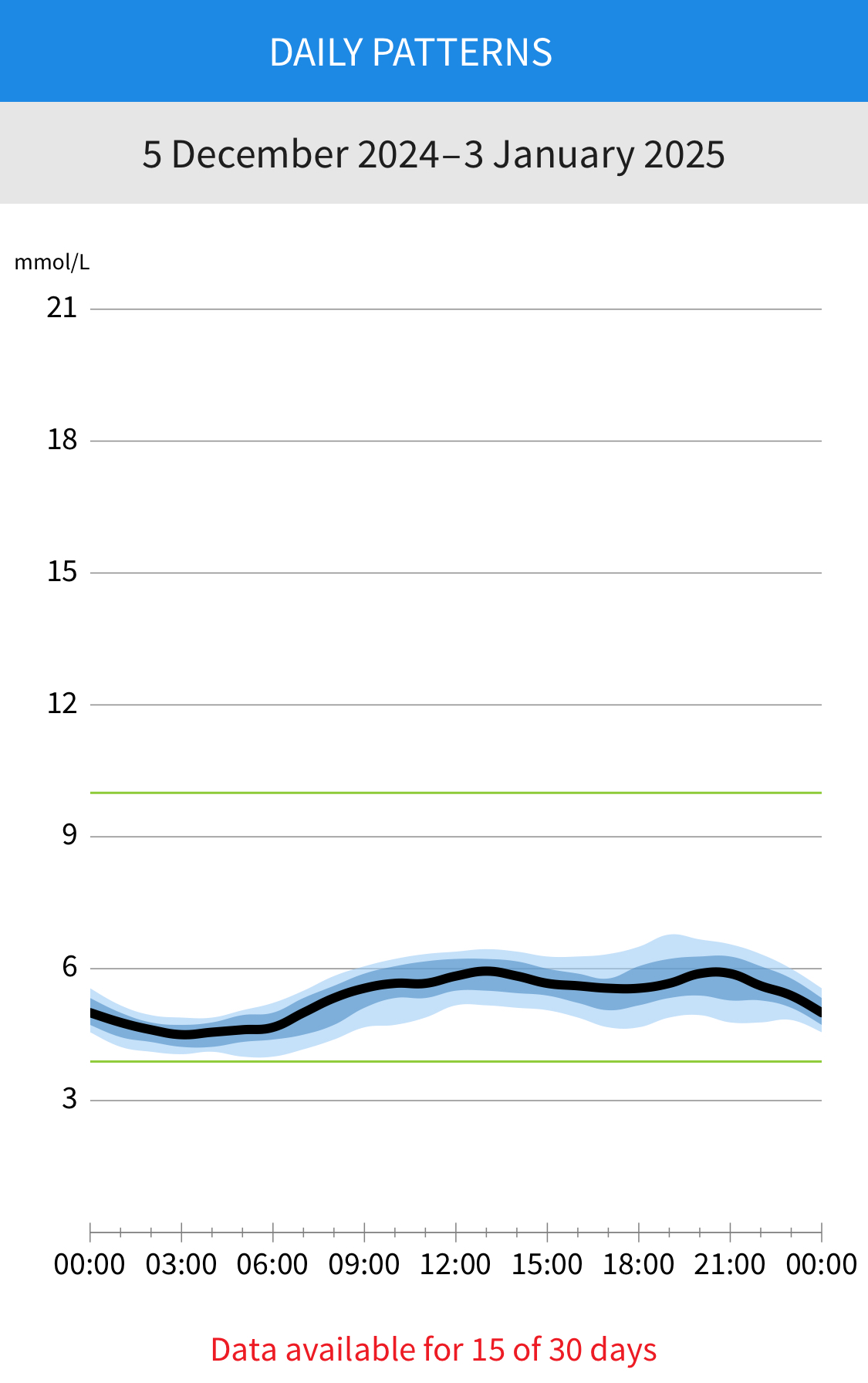 The first thing that surprised me is how tight my blood glucose range actually is. The normal range of BG readings for these purposes is 3.9 - 10 mmol/l. My highest value was 8.3 mmol/l - when I deliberately ate about 20g of sugar in chutney with lamb kebabs, for reasons that I will go into further. As it turned out, it led to a very quick spike, from 6.5 - 8.3 and back to 6.5 in an hour. Otherwise my average over the 2 weeks was between 4.5 and 6 over the course of the day. For someone who would certainly be a Type 2 diabetic by now if I had not modified my diet just over 10 years ago, I feel this chart is not too bad! The image shows the average and range of readings for the period I wore the sensor.
The first thing that surprised me is how tight my blood glucose range actually is. The normal range of BG readings for these purposes is 3.9 - 10 mmol/l. My highest value was 8.3 mmol/l - when I deliberately ate about 20g of sugar in chutney with lamb kebabs, for reasons that I will go into further. As it turned out, it led to a very quick spike, from 6.5 - 8.3 and back to 6.5 in an hour. Otherwise my average over the 2 weeks was between 4.5 and 6 over the course of the day. For someone who would certainly be a Type 2 diabetic by now if I had not modified my diet just over 10 years ago, I feel this chart is not too bad! The image shows the average and range of readings for the period I wore the sensor.
A bonus was that, being fairly meticulous with recording what I ate, I realised that I am actually eating lower levels of carbs than I thought - probably explaining why the range was tighter than I expected.
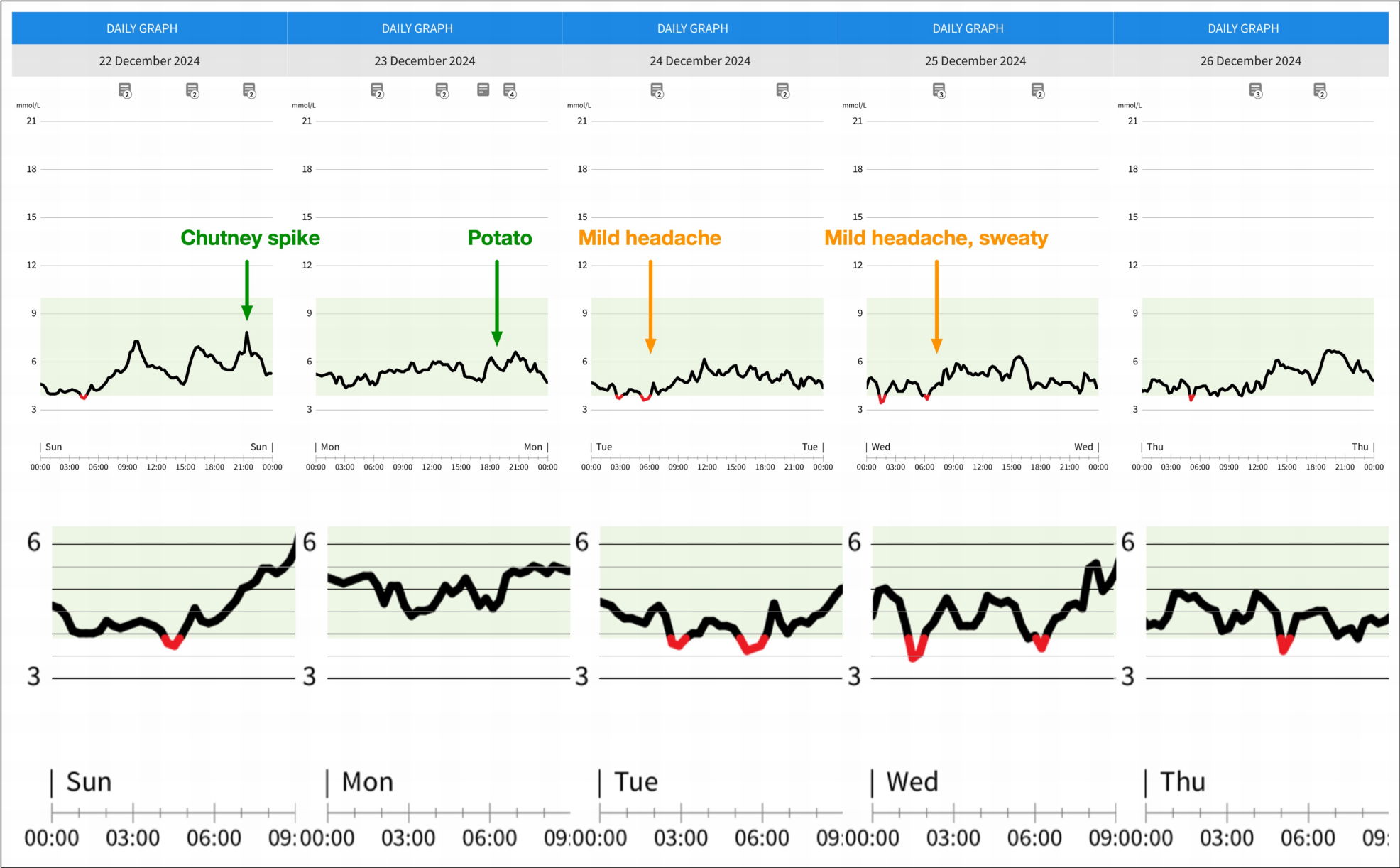
What really caught me by surprise however - and why I have delayed writing about it while I did some research - is that I had a number of very low readings during 4 nights. I say low readings rather than hypoglycaemic episodes deliberately, because the cause is not obvious, and that is what I needed to research.
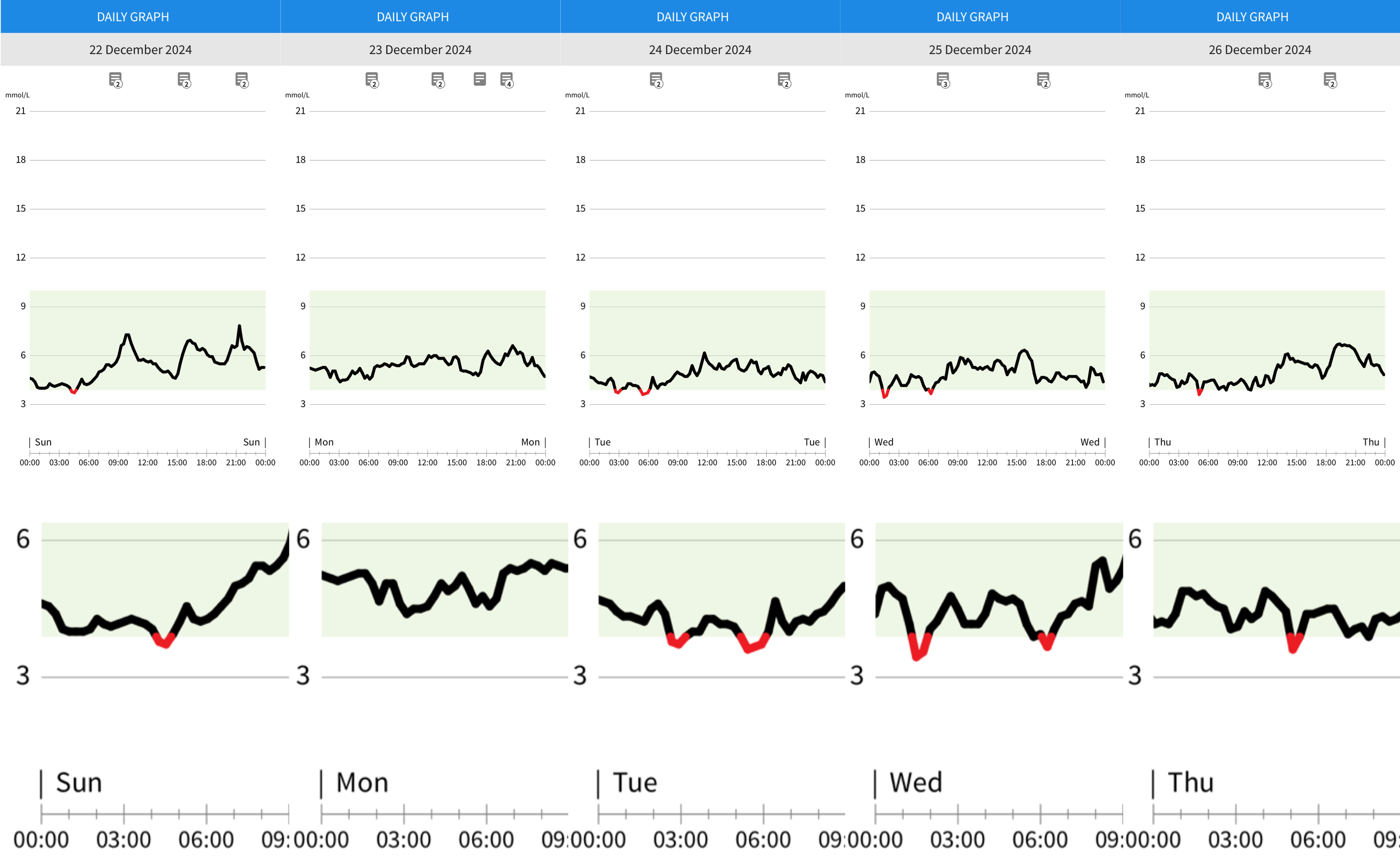
I took a closer look at the low readings - one at 04:30 in the morning of Sunday 23rd, two on the 24th (03:00 and 05:30), two on the 25th (01:30 and 06:30) and one on the 26th at 05:00.
 They did not look like typical hypos as they were very rapid onset, and short-lived. If the lows were due to nocturnal dips from diurnal variations in cortisol and glucagon, I would expect a flatter curve dipping below the low range, with a number of low readings over a longer period of time. The lowest was down to 3.4 in one case, and the longest time below 3.9 lasted about 50 minutes, with a low of 3.7 mmol/l.
They did not look like typical hypos as they were very rapid onset, and short-lived. If the lows were due to nocturnal dips from diurnal variations in cortisol and glucagon, I would expect a flatter curve dipping below the low range, with a number of low readings over a longer period of time. The lowest was down to 3.4 in one case, and the longest time below 3.9 lasted about 50 minutes, with a low of 3.7 mmol/l.
On 2 out of the 4 nights the CGM recorded lows, I woke up feeling slightly headachy, and on one slightly sweaty, both symptoms of hypos. However I had a few mornings when I had the same symptoms without having had low readings. I tried an experiment during the day to see if I had a reactive hypoglycaemia from a sugar load (hence the chutney) but it just caused a quick spike to 8.3 mmol/l and no drop afterwards.
Another thought was that it might be due tp low glycogen stores. After the low readings on Tuesday morning I tried having about 50g of potato chips - cooked with bacon fat - with dinner at 7 pm, to see if that would change anything (I know - I really didn't expect it would impact my glycogen stores). It didn’t prevent two low readings that night.
When I did some research on this, it reinforced my feeling that these were unlikely to be hypoglycaemias, and found a more likely explanation - they were caused by my sleeping position putting pressure on the sensor - i.e. I was sleeping on my arm. Studies have shown that this causes low readings due to decreased blood flow to the tissues around the sensor, and therefore a drop in glucose levels and oxygen saturation, and a rise in temperature in the interstitial fluid that the sensor measures. Both of the latter affect the sensor accuracy - low oxygen partial pressure decreasing readings and increased temperature raising the readings.
 Pressure prevention - it was neater than this when I put them on.
Pressure prevention - it was neater than this when I put them on.
So overall, it has been a very interesting and educational experience. I found the Freestyle Libre 2 worked well, although not exactly cheap at £55.99 for the 14-day sensor. The Freestyle LibreLink app worked well apart from not updating the home screen chart for an hour or so on a few occasions. I was however, very frustrated by the lack of facility to export the raw data from the Freestyle LibreLink app. This is an easy fix that they really ought to make.
Using the Freestyle LibreLinkUp and cloud-based system aimed at being able to share data with a medical practitioner/practice or other care-giver, was extremely cumbersome to implement. Again, some attention to this would pay dividends.
Further Reading:
A paper looking at the effect of body position on sensor function.
Mensh BD, Wisniewski NA, Neil BM, Burnett DR. Susceptibility of interstitial continuous glucose monitor performance to sleeping position. J Diabetes Sci Technol. 2013 Jul 1;7(4):863-70. doi: 10.1177/193229681300700408
https://pmc.ncbi.nlm.nih.gov/articles/PMC3879750
You can read about the brilliant dietician, Lily Nicol’s similar experiment, which helped inspire me to go ahead with mine. Lily is a highly respected specialist in pregnancy and pre-pregnancy nutrition, and a low carb advocate.
CGM Experiment: What I Learned as a Non-Diabetic From Wearing a Continuous Glucose Monitor
https://lilynicholsrdn.com/cgm-experiment-non-diabetic-continuous-glucose-monitor
Contact me

 What is a Low Carb Diet
What is a Low Carb Diet